Kidney stones
Highlights
Overview
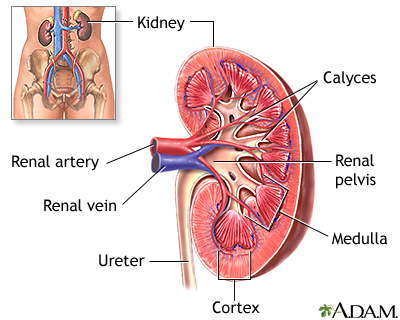
- The kidneys filter out fluids and waste from the body, producing urine. The two kidneys are located deep behind the abdominal organs, below the ribs and toward the middle of the back.
- Kidney stones are hard, solid particles that form in the urinary tract. If a stone (even a small one) blocks the flow of urine, excruciating pain may result, and prompt medical treatment may be needed.
- A CT scan is usually the best way to diagnose kidney stones and to pinpoint their location, size, and number.
Treatment
- Painful kidney stones require treatment. Depending on the type of kidney stone, dietary changes, medicines, and other noninvasive treatments are available.
- Small stones less than 5 mm usually pass on their own. In these cases, medication and dietary changes may be all that is needed.
- Larger stones, stones that are causing damage to the kidneys, or stones that do not pass on their own, usually respond well to treatments such as ureteroscopy, percutaneous nephrolithotomy (PCNL), and extracorporeal shockwave lithotripsy (SWL).
- Preventive drug therapy is matched to the exact type of stone formation. For some types of stones, this can be highly effective with a success rate of over 80%.
- A recent trial showed that percutaneous nephrolithotomy (PNL) may be an effective option for patients with moderate-size stones 10 - 20 mm in size. In the past, these patients underwent extracorporeal shockwave lithotripsy (SWL). For moderate-size stones, stone clearance was better with PNL than SWL. In addition, advances in PNL have made it similar to SWL in side effects and patient outcomes.
Introduction
Kidney stones are hard, solid particles that form in the urinary tract. In many cases, the stones are very small and can pass out of the body without any problems. However, if a stone (even a small one) blocks the flow of urine, excruciating pain may result, and prompt medical treatment may be needed.
Urine is formed in the kidneys. The kidneys filter out fluids and waste from the body, producing urine. As the urine passes through the kidneys, it becomes more concentrated. From the kidneys, urine flows through thin tubes called ureters into the bladder. The bladder's stretchy walls expand to store the incoming urine until it leaves the body through a tube called the urethra.
The two kidneys are located deep behind the abdominal organs, below the ribs and toward the middle of the back.
Types of Kidney Stones
Occasionally, high levels of chemicals in the urine form into crystals. Eventually these crystals become large enough to form stones in the kidney, a condition called nephrolithiasis. Stones (calculi) may also form in the ureter or the bladder. Combinations of minerals and other chemicals, some derived from a person's diet, make up the salts in these stones.
Calcium Stones. About 80% of all kidney stones contain calcium, usually combined with oxalate, or oxalic acid. Many common vegetables, fruits, and grains contain oxalate.
A smaller percentage of calcium stones are made of calcium phosphate (called brushite).
Uric Acid Stones. Uric acid is responsible for almost 10% of kidney stones. It is the breakdown product of purines, nitrogen compounds found in the body and in certain foods. Uric acid enters the bloodstream, and then passes primarily into the kidneys. From the kidneys, uric acid leaves the body in the urine. Often, uric acid stones occur with calcium stones.
Struvite Stones. Struvite stones are made of magnesium ammonium phosphate. They are almost always associated with certain urinary tract infections. Worldwide, they account for up to 30% of all kidney stones. In the United States, however, fewer than 15% of all stones are struvite. Most struvite stones occur in women. The rate of these stones may be declining in America, perhaps because of better control of urinary tract infections.
Cystine Stones. A buildup of the amino acid cystine, a building block of protein, causes 1% of kidney stones in adults and up to 8% of stones in children. The tendency to form these stones is inherited. Cystine stones grow rapidly and tend to recur. If not treated promptly, they can eventually lead to kidney failure.
Xanthine Stones. Other kidney stones are composed of xanthine, a nitrogen compound. These stones are extremely uncommon and usually occur as a result of a rare genetic disorder.
Causes
The key process in the development of kidney stones is supersaturation.
- The urine carries chemicals, including calcium oxalate, uric acid, cystine, or xanthine.
- These substances can become extremely concentrated if there is not enough urine, or if unusually high amounts of crystal-forming salts are present.
- When the chemical concentration levels reach the point at which they no longer dissolve, these substances form crystals.
Different factors may be involved in either reducing the volume of urine, or increasing the amount of chemicals.
Deficiencies in Protective Factors. Normally, urine contains substances that protect against stone formation, including:
- Magnesium
- Citrate
- Pyrophosphate
- Enzymes
These substances:
- Allow chemicals in the urine to be at high concentrations without forming crystals
- Prevent crystal formation
- Coat the crystals and prevent them from sticking to the surface of kidney tubes
Not having enough of these protective substances can cause stones.
Changes in the Acidity of the Urine. Changes in the acid balance of the urine can affect stone formation.
- Uric acid and cystine stones mainly form in acidic urine.
- Calcium phosphate and struvite stones increase in alkaline urine.
Causes of Calcium Stones
Often, the cause of calcium stones is not known. The condition is then called idiopathic nephrolithiasis. Research suggests that nearly all stones result from problems in the breakdown and absorption of calcium and oxalate. Genetic factors may play a role in about half of these cases. Many medical conditions and drugs can also affect digestion and intestinal absorption.
Excess Calcium in the Urine (Hypercalciuria). Hypercalciuria (too much calcium in the urine) is responsible for as many as 70% of calcium-containing stones. A number of conditions may produce hypercalciuria. Many are due to genetic factors, but most cases are due to unknown causes (idiopathic).
The following can lead to hypercalciuria and calcium stones:
- Too much calcium absorbed by the intestines. This is usually caused by genetic factors.
- Excessive chloride. Chloride has a negative charge and calcium has a positive charge, so they balance each other in the body. Excess chloride may lead to excess calcium.
- Renal calcium leak. In this condition, the kidney does not regulate minerals normally, causing an increase of calcium in the urine.
- Excessive sodium. High urinary levels of sodium result in increased levels of calcium. Certain defects in the kidney tubules transport system cause imbalances in sodium and phosphate, which can lead to high calcium levels in the urine. A high-salt diet can also produce this effect.
Excess Oxalate in the Urine (Hyperoxaluria). Oxalate is the most common stone-forming compound. Too much oxalate in the urine is responsible for up to 60% of calcium stones and is a more common cause of stones than excess calcium in the urine.
Hyperoxaluria can be either primary or secondary.
- Primary hyperoxaluria is an inherited disorder in which too much oxalate in the urine is the main problem.
- Secondary hyperoxaluria results from specific conditions that cause high levels of urinary oxalate.
Secondary hyperoxaluria is usually caused by too much dietary oxalates (found in a number of common vegetables, fruits, and grains) or by problems in the body's breakdown of oxalates. Such defects may be due to various factors:
- Severe vitamin B6 deficiencies (usually due to genetic disorders)
- Deficiencies in Oxalobacter formigenes, an intestinal bacteria that breaks down oxalate
- Short bowel syndrome, a condition that generally occurs when portions of the small intestines are removed. It causes an inability to properly absorb fat and nutrients. Calcium may bind to the unabsorbed fat instead of to the oxalates, which causes a buildup of oxalate.
- Androgens (male hormones)
Female hormones (estrogens) actually lower the risk of hyperoxaluria. Estrogen may help prevent the formation of calcium oxalate stones by keeping urine alkaline, and by raising protective citrate levels.
Patients who undergo the most common type of gastric bypass surgery, the Roux-en-Y, may be at increased risk for calcium oxalate kidney stones beginning 6 months after surgery. The added kidney stone risk is thought to be due to changes in the urine. Patients who have undergone Roux-en-Y gastric bypass surgery have excess oxalate and low levels of citrate in their urine after the procedure.
Another type of weight loss surgery, gastric banding, does not appear to increase the risk for kidney stones.
Excessive Calcium in the Bloodstream (Hypercalcemia). Hypercalcemia generally occurs when bones break down and release too much calcium into the bloodstream. This is a process called resorption. It can occur from several different diseases and events:
- Hyperparathyroidism. Overactive parathyroid glands cause about 5% of calcium stones. People with this disorder have at least a 20% chance of developing kidney stones. Women are more likely to have this disorder than men.
- Immobilization. Lack of movement can lead to kidney stones.
- Renal tubular acidosis. This disorder causes an acid and alkaline imbalance. Renal tubular acidosis not only increases calcium levels in the bloodstream, but it also reduces protective citrate levels.
Hyperuricosuria is a condition in which there are high levels of uric acid in the urine. It occurs in 15 - 20% of people (mostly men) with calcium oxalate stones. Urate, the salt formed from uric acid, creates the center of a crystal (nidus), around which calcium oxalate crystals form and grow. Such stones tend to be severe and recurrent. They appear to be strongly related to a high intake of protein. (Hyperuricosuria also plays a major role in some uric acid stones.)
Low Urine Levels of Citrate (Hypocitraturia). Citrate is the main substance in the body that is responsible for removing excess calcium. It also blocks the process that turns calcium crystals into stones. Low levels of citrate in the urine is a significant risk factor for calcium stones. Hypocitraturia also increases the risk for uric acid stones. This condition most likely contributes to about a third of all kidney stones.
Many conditions can reduce citrate levels, including:
- Renal tubular acidosis
- Potassium or magnesium deficiency
- Urinary tract infection
- Kidney failure
- Chronic diarrhea
Low Levels of Other Stone-Blocking Compounds. Several other compounds in the urine, including magnesium and pyrophosphate, also prevent the formation of calcium stones. If any of these compounds are lacking, stones may develop.
Causes of Uric Acid Stones
Human body tissues, and certain foods, contain substances called purines. Purine-containing foods include dried beans, peas, and liver. When the body breaks down purines, it produces uric acid. The presence of a certain level of uric acid in the body is normal, but excess uric acid can lead to stones.
The following conditions are usually seen in patients with uric acid stones:
- Too much uric acid in the urine for a long period of time (the most important cause of uric acid stones)
- Lower-than-normal amounts of urine produced
- Hyperuricosuria, a metabolic disorder that leads to high levels of uric acid in the urine
Note: Hyperuricosuria can also trigger calcium stones. Therefore, patients with hyperuricosuria may have a combination of calcium and uric acid stones.
Many conditions and other factors may contribute to, or cause, uric acid stones:
- Gout. Uric acid and other kidney stones develop in up to 25% of patients with primary gout, a painful form of arthritis that occurs when uric acid in the blood forms crystals in one or more joints.
- Diabetes. People with type 2 diabetes have highly acidic urine that can lead to kidney stones, particularly uric acid stones.
- Insulin resistance. People with insulin resistance have an increased risk for uric acid stones. The reason is unknown, but it may be related to the transport of certain salts through the kidneys. This transport changes in patients with insulin resistance.
- Kidney abnormalities. Kidney problems that reduce the production of ammonia, particularly in people with diabetes or insulin resistance, may lead to the formation of uric acid stones.
- Genetic factors. Inherited factors can increase a person's risk for uric acid stones.
- Hypocitraturia. Hypocitraturia is a low amount of citrate in the urine.
- Diet. Eating too much animal protein increases the risk of forming uric acid stones.
Other risk factors include:
- Certain medications (such as chemotherapy drugs, diuretics, and salicylates)
- Binge drinking
- Not eating for long periods of time (fasting)
- Lead poisoning
- Treatment for blood cancers (such as leukemia, multiple myeloma, and lymphomas)
- Some rare types of anemia (low levels of red blood cells in the blood)
- Chronic diarrhea
Causes of Struvite Stones
Struvite stones are almost always caused by urinary tract infections. Bacteria produce certain enzymes, which raise the concentration of ammonia in the urine. Ammonia makes up the crystals that form struvite stones. The stone-promoting bacteria are usually Proteus, but they may also include Pseudomonas, Klebsiella, Providencia, Serratia, and Staphylococcus. Women are twice as likely to have struvite stones as men.
Causes of Other Stones
Other stones, including cystine and xanthine stones, are usually due to genetic abnormalities.
Causes of Cystine Stones. Cystine stones develop from genetic defects that cause the abnormal transport of amino acids in the kidney and gastrointestinal system, leading to a buildup of cystine. Researchers have identified two genes responsible for this condition: SLC3A1 and CLC7A9.
Causes of Xanthine Stones. In some cases, xanthine stones may develop in patients being treated with allopurinol for gout.
Risk Factors
Kidney stones are one of the most common disorders of the urinary tract. They are an ancient health problem. Evidence of kidney stones has been found in an Egyptian mummy estimated to be more than 7,000 years old.
At this time, studies suggest that kidney stones affect more than 5% of Americans, and the rate has increased since the 1970s. People who form kidney stones appear to be at increased risk for certain other disorders, including heart attacks.
Gender and Age
Men. Kidney stones are two times more common in men than women, but the likelihood of stones is increasing in both men and women. The risk of kidney stones increases in men in their 40s and continues to rise until age 70. By age 70, 11% of men will have had a kidney stone that causes symptoms. Caucasian men have a higher risk than other ethnic groups.
Women. The risk of kidney stones peaks in a woman's 50s. In younger women, stones are more likely to develop during the late stages of pregnancy. Pregnant women tend to have a higher calcium intake, but their kidneys do not handle the calcium as well as they did before pregnancy. Kidney stones are still rare during pregnancy, however, affecting only 1 in 1,500 pregnancies.
Risk Factors in Children. Stones in the urinary tract in children are usually due to genetic factors. Most of the time, the cause is too much calcium in the urine (hypercalciuria). Deformities in the urinary tract pose a significant risk for kidney stones in children. Babies born at a low birth weight who need to be fed intravenously are also at risk for stones.
Rates of kidney stones in adolescents have doubled in the last 25 years. Although researchers don't know the exact reason for this increase, they think it may have to do with body weight, which has been rising in young people over the years.
Obesity and Weight Gain
Obesity and weight gain are both associated with an increased risk for kidney stones.
Higher BMIs and larger waist circumferences are both risk factors for kidney stones. Researchers think that there may be a link between fat tissue, insulin resistance, and urine composition. People with larger body sizes may excrete more calcium and uric acid into the urine, which increases the risk for kidney stone formation.
Family History
Having a family history of kidney stones doubles a person's risk for the condition. Researchers are looking into genetic markers or other factors that might predict the risk of kidney stones in relatives, although none has yet been clearly identified. A family history of gout may also make a person more vulnerable to developing stones.
Ethnicity
Caucasians seem to have the highest incidence of kidney stones, followed by Mexican Americans. African-Americans have the lowest risk. Caucasians are three times more likely to form kidney stones than African-Americans. Dietary
factors can diminish any protective effects of ethnicity however.
Geographical Differences
Dietary factors, minerals in local water, or both may contribute to geographic differences that have been observed in the occurrence of kidney stones. Studies have reported the highest occurrence of kidney stones in the southern region of the United States and the lowest occurrence in the western region.
Lifestyle Factors
Specific Foods. In general, certain foods increase the risk for stones, but only in people who have a genetic or medical vulnerability. People whose diets are high in animal protein and low in fiber and fluids may be at higher risk for stones. A number of foods contain oxalic acid, but there is no proof that such foods make any major contribution to calcium oxalate stones in people who do not have other risk factors. However, several studies have shown that increasing dietary calcium and restricting salt, animal protein, and foods rich in oxalate can help prevent calcium oxalate stones from returning.
Stress. One study reported that people who had a major, stressful life experience were more likely to develop stones than those who had not had a stressful experience. Some experts speculate that this increased risk may be due to a hormone called vasopressin, which is released in response to stress. Vasopressin also decreases the volume of urine, which makes the chemicals in urine more concentrated and prone to forming crystals and stones.
Being Bedridden. Any medical or physical condition that keeps a person in bed or immobile increases blood levels of calcium from bone breakdown, thereby posing a risk for stone formation.
Medical Conditions
Gout. Patients with gout are at high risk for uric acid stones.
High Blood Pressure. People with high blood pressure are up to three times more likely to develop kidney stones. It is not entirely clear whether having high blood pressure increases the risk for a stone, stones lead to high blood pressure, or there is a factor linking both conditions.
Inflammatory Bowel Disease. Crohn's disease and ulcerative colitis cause problems in the absorption of substances in the intestines. These problems significantly increase the risk for kidney stones, particularly in men.
Urinary Tract Infections. Urinary tract infections (UTIs) are almost always the cause of struvite stones.
Hyperparathyroidism. The parathyroid glands regulate calcium levels in the body through parathyroid hormone. In hyperparathyroidism, one or more of these glands makes too much parathyroid hormone. Some people with hyperparathyroidism develop kidney stones. Surgery to remove the hyperactive parathyroid gland in such patients reduces the risk for stone formation, but the risk still remains high for some time after surgery.
Other Medical Conditions. Diabetes, kidney disease, chronic diarrhea, certain cancers (such as leukemia and lymphoma), and sarcoidosis (a type of inflammation in lymph nodes and other tissues) put people at higher risk for stones.
Medications
AIDS medications. More than 10% of AIDS patients who take the medicine indinavir develop stones. The risk is even higher in people with AIDS who also have hepatitis B, hepatitis C, or hemophilia, as well as those who are very thin or who take the antibiotic combination TMP-SMX.
Other Drugs. Kidney stones are a rare side effect of thyroid hormones and loop diuretics (drugs that increase urination), although diuretics are also used to prevent calcium stones. Certain cancer chemotherapy drugs can also cause kidney stones. Long-term use of medications such as antacids, which change the acid content of urine, may increase the risk for kidney stones.
Ephedrine (found in some drugs used to treat asthma and congestion), triamterene (sometimes used to treat high blood pressure and fluid build-up), magnesium antacids (silicates), sulfamethoxazole-trimethoprim (used to treat certain infections), topiramate (used to treat certain seizures), carbonic anhydrase inhibitors (used to treat glaucoma), furosemide (used to treat high blood pressure or fluid retention), vitamin C or D excess, and laxatives may also provoke kidney stones.
Symptoms
In many cases, kidney stones do not produce symptoms. However, if a stone becomes trapped (or lodged) in the ureter (the thin tube between the bladder and kidney), symptoms can be very severe. Often, symptoms vary depending on the stone's location and its progress.
Kidney stone attacks tend to be most common late at night or in the early morning, possibly because of low urine output during these times. Kidney stone attacks are least common during the late afternoon.
- Pain usually begins abruptly on one side and then continues to be intense and consistent. (In some cases it lasts for a few minutes, disappears, then returns after about 10 minutes.)
- The patient cannot find a comfortable position and usually stands, sits, paces, or reclines in a failed search for a position that will bring relief.
- If the stone is in the kidney or upper urinary tract, the pain usually starts in one flank area (to the side of the back near the waist). It typically radiates to the groin.
- If the stone is too large to pass easily, the pain follows the muscle contractions in the wall of the ureter as they try to squeeze the stone along into the bladder.
- Nausea and vomiting may occur.
- Blood may be present in the urine.
- As the stone passes down the ureter, closer to the bladder, the person may feel the need to urinate more often or a burning sensation during urination.
- A fever suggests that the person may also have a urinary tract infection.
The size of the stone does not necessarily predict the severity of the pain. A very tiny crystal with sharp edges can cause intense pain, while a larger round stone may not be as distressing. Struvite stones can often occur without symptoms.
Diagnosis
The doctor will perform a physical exam. This includes tapping on the back over the kidneys and pressing on the abdomen to detect tender locations.
Medical History
The patient's age is a significant factor. Kidney stones that occur in children and young patients are more likely to result from inherited problems that cause excess cystine, xanthine, or, in some cases, calcium oxalate. In adult patients, calcium stones are most common.
A medical history may help predict which crystal has formed the stone. The doctor will need to know the following:
- Any previous kidney stone attacks
- History of cancer, sarcoidosis, or small bowel disease
- Any medications being taken, including non-prescription substances, particularly high doses of vitamins D or C and calcium-containing antacids
Ruling out Other Disorders
Many conditions can cause symptoms similar to those of kidney stones. Usually the diagnosis is easily made because of the type of symptoms, but it is not always clear. Urinary tract infections can cause similar, but usually less intense, pain. In fact, people with an infection may also have a kidney stone.
Other causes of pain that may mimic kidney stones include:
- Gallstones
- Diverticulitis (infection or irritation of abnormal pouches in the intestines)
- Intestinal blockage
- Blood clots
- Irritable bowel syndrome
- Appendicitis
- Peptic ulcers
- Pancreatitis (inflammation of the pancreas)
- Hepatitis
- Pelvic inflammatory disease
- Inflammatory bowel disease (Crohn's and colitis)
- Heart attack
Imaging Techniques
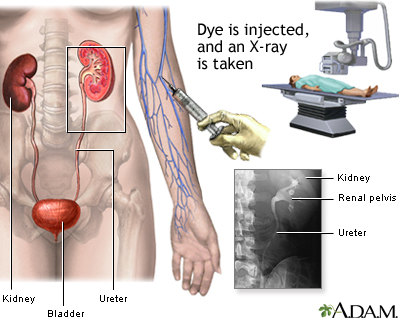
Various imaging techniques are helpful in determining the presence of kidney stones. The best approach uses spiral (or helical) computed tomography (CT) scans. If these scans are not available, the patient will need ultrasound or standard x-rays. If no stones show up, but the patient has severe pain that suggests the presence of kidney stones, the next step is an intravenous pyelogram (IVP).
X-Rays. A standard x-ray of the kidneys, ureters, and bladder may be a good first step for identifying stones, because many stones are visible on x-rays. Calcium stones can be identified on x-rays by their white color. Cystine crystals can also show up on x-rays.
Computed Tomography. A type of CT scan called a spiral or helical CT scan is currently the best method for diagnosing stones in either the kidneys or the ureters. CT scans can be used to find the exact location of the stone, as well as to look for anatomical problems that may have led to stone formation. This test is fast, noninvasive, and it provides detailed, accurate images of even very small stones. If stones are not present, a spiral CT scan can often identify other causes of pain in the kidney area. It is better than x-rays, ultrasound, and IVP for detecting kidney stones. Experts hope spiral CT will eventually be able to identify the chemicals present in a stone.
Ultrasound. Ultrasound can detect uric acid stones and blockages in the urinary tract. It is not useful for finding very small stones, but some research indicates that it may be an effective first diagnostic step in the emergency room to help identify whether a patient has a stone. Ultrasound is also effective in children.
Intravenous Pyelogram (IVP). With IVP, the doctor injects a special dye into the patient. A technician then takes x-rays as the dye enters the kidneys and travels down the urinary tract. IVP is invasive but, until recently, it was the most cost-effective method for detecting stones. Where it is available, spiral CT is now preferred, since it gives a faster diagnosis and is more accurate, safer, and similar in cost.
IVP should not be used on patients with kidney failure. There is also a risk for an allergic reaction to standard dyes, although newer, less allergenic dyes are becoming available.
Magnetic Resonance Imaging. Magnetic resonance imaging (MRI) techniques are showing promise for diagnosing urinary tract obstruction, but they do not yet accurately reveal small stones, or stones that do not cause a blockage. Because no radiation is involved with MRIs and ultrasounds, however, they are good options for children and pregnant women.
Urine Tests
Urine samples are needed to evaluate features of the urine, including its acidity and the presence of:
- Red or white blood cells
- Infection
- Crystals
- High or low levels of chemicals that inhibit or promote stone formation
Clean-Catch Urine Sample for Culturing. After determining that a kidney stone is present, the health care provider usually gives the patient a collection kit, including filters, to try to catch the stone or gravel as it passes out. The urine may also be tested (cultured) for the presence of infection-causing organisms. A clean-catch urine sample is almost always required for culturing. To provide a clean catch, do the following:
- First, wash your hands thoroughly, and then wash the penis or vulva and surrounding area four times with downward strokes, using a new soapy sponge each time.
- Begin urinating into the toilet and stop after an ounce or two.
- Position the container to catch the middle portion of the urine stream.
- Urinate the remainder into the toilet.
- Tighten the cap on the container securely, being careful not to touch the inside of the rim.
Twenty-Four Hour Urine Collection. A 24-hour urine collection may be needed to measure urine volume and levels of acidity, calcium, sodium, uric acid, oxalate, citrate, and creatinine.
- You should not change any of your usual eating or drinking patterns when performing this test.
- Discard the first urination on the day of the test.
- Afterward, collect all urine passed over the next 24 hours, including the first urination on the morning of the second day.
- A second 24-hour urine collection may be needed to determine whether treatment is working, or it may be done if the first analysis was not conclusive and the doctor suspects a less common stone, such as a cystine or xanthine stone.
Urine tests that are used to determine the specific chemical and biological factors causing the stone should be performed about 6 weeks after the attack, since the attack itself may change the levels of such substances, including calcium, phosphate, and citrate.
Note that calcium levels in the urine may be abnormal even in many people who do not have stones. In addition, high urinary concentrations of calcium may pose a greater or lesser risk for stones, depending on a person's age.
Microscopic Examination
Kidney stones that are removed are sent for stone analysis (crystallography).
Testing the Acidity of Urine
Testing whether urine is acidic or alkaline helps to identify the specific type of stone. The levels of acidity or alkalinity in any solution, including urine, are indicated by the pH scale:
- A pH value of 7.0 is neutral.
- A solution with a low pH (below 7.0) is acidic. (A low pH favors the development of uric acid and cystine stones.)
- A solution with a high pH is alkaline. (A high pH favors the development of calcium phosphate and struvite stones.)
Testing for Blood in the Urine
A dipstick test for blood in the urine (called hematuria) is typically performed when patients come to the emergency room with flank pain (the primary symptom of kidney stones). About a third of kidney stone patients do not show blood in the urine, so other tests may be needed.
Blood Tests
Blood Tests for Stone Factors. Blood and urine tests help determine what substances formed the crystals. This allows the doctor to determine the appropriate treatment and preventive measures.
Blood tests may help determine blood levels of urea nitrogen, creatinine, calcium, phosphate, and uric acid in patients with known or suspected calcium oxalate stones. Doctors will usually schedule these tests about 6 weeks after the attack, in order to measure these substances when the stone has been passed and the patient has been stabilized. This is particularly true in patients with recurrent stones.
Parathyroid Tests. Tests to detect parathyroid hormone levels are given if the doctor suspects hyperparathyroidism based on other signs and symptoms.
Tests for Infection. A test result that shows a high white blood cell count might indicate infection. Such results, however, could be misleading, since the number of white blood cells could also increase in response to the extreme physical stress of a kidney stone attack.
Tests for Metabolic Problems. About half of children with stones have an identifiable metabolic disorder, which increases their risk of stone recurrence five-fold. Experts argue whether tests for metabolic disorders are routinely needed once the stone composition has been determined. Studies suggest the following:
- People with recurrent calcium stones have a wide range of irregular blood or urine test results, indicating a variety of possible metabolic disorders. For example, calcium stones in middle-aged women may be due to parathyroid abnormalities.
- Calcium phosphate stones most likely result from renal tubular acidosis.
- People with non-calcium stones generally have identifiable metabolic disorders.
- Determining the stone composition may be sufficient for treatment, and may help avoid unnecessary metabolic tests.
Treatment
When tests show someone has a kidney stone, the next step is to determine treatment. Patients who have severe pain, vomiting, fever, or symptoms of infection should be evaluated and treated in the emergency room. The size, location, type, and number of stones are important factors in determining the best treatment.
Treatment for Severe Attacks
Strong opioid painkillers are often required for a severe kidney stone attack. However, doctors will usually not give such drugs until they confirm the presence of a kidney stone with an imaging study.
Watchful Waiting
In about 85% of patients, the kidney stones are small enough (about 5 mm) that they pass through normal urination, usually within 2 - 3 days. In some cases, a stone may take weeks to months to pass, although the pain usually goes away before that.
The patient should drink plenty of water (2 - 3 quarts a day) to help move the stone along, and take painkillers as needed. The doctor usually provides a collection kit with a filter and asks the patient to save any passed stones for testing.
If the stone has not passed in 2 - 3 days, the patient will need additional treatments. In some severe cases, hospitalization may be necessary.
Alpha blockers (such as tamsulosin) can relax muscles in the urinary tract, helping kidney stones pass.
Treatment by Stone Type | |||
Stone Type | Diet and Lifestyle | Medications | Procedures |
Calcium Oxalate | Plenty of fluids. (Choose water, lemon juice. Avoid grapefruit, apple, and cranberry juice.) Limit the amount of protein and salt in the diet. Increase fiber. Limit the amount of fats in the diet, particularly in people who have short bowel syndrome. Balance normal calcium intake with potassium- and phosphate-rich foods. Limit the amount of calcium in the diet (only in people who have genetic abnormalities that cause high intestinal absorption of calcium). Limit the amount of foods high in oxalates (only in patients with rare intestinal conditions that cause hyperoxaluria). | Diuretics ("water pills"), citrate salts, phosphates, cholestyramine | Lithotripsy, uteroscopy, percutaneous nephrolithotomy, open surgery |
Uric Acid | Plenty of fluids. (Choose water, blackcurrant juice. Avoid cranberry juice.) Increase calcium intake (be sure it is well-balanced with potassium and phosphates and taken with food). Reduce protein and other foods with high purine content. | Potassium citrate, sodium bicarbonate, allopurinol | Lithotripsy, uteroscopy, percutaneous nephrolithotomy, open surgery |
Struvite stones | Plenty of fluids (water, cranberry juice) Reduce proteins | Antibiotics to eliminate any infection. Acetohydroxamic acid (AHA) may be helpful in combination with antibiotics. In some cases, organic acids are given through the urinary tract. | May respond poorly to most lithotripsy procedures and require open surgery. Newer procedures may be helpful. |
Cystine stones | Very high fluid intake (4 quarts a day) Limit the amount of protein in the diet. | Alkalizing agents (such as bicarbonate). Sometimes d-penicillamine, tiopronin, or captopril is useful for lowering cystine levels. | May respond poorly to most lithotripsy procedures and require open surgery. Newer procedures may be helpful. |
Medications
Medications for Calcium Stones
Diuretics. Diuretics are medicines commonly used to treat high blood pressure and other disorders. They remove fluid and sodium from the body. Low doses of a class of diuretics known as thiazides are sometimes used to reduce the amount of calcium the kidneys release into the urine. Thiazides include:
- Hydrochlorothiazide (Esidrix, HydroDIURIL)
- Chlorothiazide (Diuril)
- Trichlormethiazide (Metahydrin, Naqua)
- Chlorthalidone (Hygroton)
However, thiazides also cause potassium loss, which reduces citrate levels and can increase the risk for stones. Patients taking thiazide pills may also take potassium citrate to prevent citrate loss. Amiloride (Midamor) is a potassium-sparing diuretic, which may be used if a thiazide does not work. Thiazides may cause muscle cramps.
Citrates. Citrate salts are often given to people with calcium oxalate or uric acid stones:
- Potassium magnesium citrate is available over the counter. It is proving to be very beneficial in preventing kidney stones.
- Potassium citrate (such as K-Lyte, Polycitra-K, and Urocit-K) is the only treatment given to people with normal urine calcium levels. Between 70 - 75% of patients with recurrent stones have ongoing remission (no stone recurrence) with potassium citrate treatment. However, some people cannot tolerate potassium citrate because of side effects (stomach problems).
- Magnesium citrate (such as Citroma and Citro-Nesia) may help people who develop calcium stones from impaired intestinal absorption due to short bowel disease.
Citrates may cause stomach upset. People with struvite stones, urinary tract infections, bleeding disorders, or kidney damage should not use these products. Patients who take citrate supplements containing potassium should not take any other medications that contain potassium or prevent its loss (such as potassium-sparing diuretics). People with peptic ulcers should avoid citrate supplements, or discuss using non-tablet forms with their doctor.
Phosphates. Phosphates help reduce the breakdown of bone that releases calcium into the bloodstream. They are also involved in the kidney's reabsorption of calcium from the urine.
Phosphate compounds:
- Neutral (nonacidic) sodium or potassium phosphate (such as K-Phos, Neutral, and Neutra-Phos) is usually taken four times a day after meals to prevent kidney stones. Diarrhea is a possible side effect.
- Cellulose phosphate (Calcibind) is recommended only for severe hypercalciuria that is associated with recurrent calcium stones and caused by excessive absorption of calcium from the intestines. This drug may increase oxalate levels and decrease magnesium levels, which can lead to different kinds of stones. Taking magnesium supplements and reducing dietary oxalates, calcium, and ascorbic acid may help offset these risks. Cellulose phosphate may also cause bloating.
Avoid acidic forms of phosphate, because they increase the risks for both hypocitraturia and hypercalciuria. They may cause gastrointestinal distress.
Cholestyramine (such as Questran and Questran Light) is a drug used to reduce cholesterol levels. However, because it binds with oxalate in the intestine, it is also used to reduce high oxalate levels in urine (hyperoxaluria). The drug usually comes in a powder that is dissolved in liquid. Bloating and constipation are common side effects of this drug. Cholestyramine also interferes with other medications, including digoxin (Lanoxin) and warfarin, and it may contribute to calcium loss and osteoporosis. In order to prevent such interactions, take other drugs 1 hour before, or 4 - 6 hours after taking cholestyramine.
Long-term use of cholestyramine may cause deficiencies of vitamins A, D, E, and K. Vitamin supplements may be necessary.
Medications for Uric Acid Stones
Sodium Bicarbonate. Patients whose persistently acidic urine causes uric acid stones may take sodium bicarbonate to reduce urine acidity. Patients taking sodium bicarbonate must test their urine regularly with pH paper, which turns different colors depending on whether the urine is acidic or alkaline. Too much sodium bicarbonate can cause the urine to become too alkaline. This increases the risk for calcium phosphate stones. Patients who need to reduce the amount of sodium they take in (as a result of other medical conditions) should not use sodium bicarbonate.
Potassium Citrate. Potassium citrate, which restores citrate to the urine, is useful for patients with high levels of uric acid in the urine.
Allopurinol. Allopurinol (Lupurin, Zyloprim) is very effective at reducing high blood levels of uric acid, and it may be helpful for patients with uric acid stones. Allopurinol will not prevent calcium stones from forming. There is also a slight risk for the formation of xanthine stones with this drug. Side effects include diarrhea, headache, muscle pain, and fever. About 2% of patients have an allergic reaction to allopurinol that causes a rash. In rare cases, the rash can become severe and widespread enough to be life threatening.
Allopurinol reduces uric acid levels rapidly, so it may trigger an attack of gout in vulnerable people. To prevent this problem, patients taking allopurinol should also take a nonsteroidal anti-inflammatory drug (NSAID) for 2 or 3 months. Aspirin should not be taken, because it increases uric acid levels. Patients should discuss the appropriate NSAID choice with their doctor.
In 2009, the U.S. Food and Drug Administration (FDA) approved febuxostat (Uloric) to treat gout. It is the first new treatment for gout in 40 years. Febuxostat lowers uric acid levels by inhibiting the same enzyme as allopurinol. Patients who are allergic to allopurinol can take febuxostat This new drug is very effective, but expensive.
Medications for Struvite Stones
Before patients can receive any medical treatment for struvite stones, they must have surgery to completely remove the stones.
Antibiotics for Eliminating Infection. People with struvite stones should receive ongoing treatment with antibiotics to keep the urine free of the bacteria that cause urinary tract infections. Careful follow-up and urine testing are extremely important. A high urine pH indicates low acidity and an increased risk for infection.
Acetohydroxamic Acid (AHA). Acetohydroxamic acid (AHA or Lithostat) is beneficial when used with long-term antibiotics. AHA blocks enzymes that bacteria release, and it has been effective in preventing stones even when bacteria are present. Side effects, however, can be severe. The drug reduces iron levels in the body, so anemia is a common problem. Patients may need to take iron supplements. Other side effects include nausea, vomiting, depression, anxiety, rash, persistent headache, and, rarely, small blood clots in the legs. This drug is recommended only for patients with healthy kidneys whose condition is due to specific struvite-causing organisms. Patients taking this medicine should avoid alcohol. Pregnant women should not take acetohydroxamic acid.
Organic Acids. Medical treatments to dissolve stones may be useful in patients who do not respond to other medications, or in combination with surgery. Acidic urine dissolves struvite stones, so the doctor may wash the urinary tract with a solution of organic acids (such as Renacidin). Candidates for such washes must have sterile urine (no bacteria or other organisms in the urine) and healthy kidney function. In surgical patients, the wash is performed 4 or 5 days after the operation. The wash starts with saline (salt solution) for 1 - 2 days and, if there are no problems, the organic acid solution follows for another 1 or 2 days, until all stones dissolve. Regular urine tests are necessary to ensure that the bacteria do not return.
Aluminum Hydroxide Gel. An aluminum hydroxide anti-acid gel may reduce the phosphate levels that contribute to struvite stone formation, but it has a long-term risk of causing aluminum toxicity. Long-term reduction of phosphorus can also increase the risk for calcium oxalate stones. Experts recommend limiting phosphorus through a low-protein diet, rather than with this gel.
Medications for Cystine Stones
The first-line treatment for cystine stones is increasing the alkalization of urine so the stones can dissolve. If alkalization fails, drug treatments may include d-penicillamine, alpha-mercaptopropionylglycine (tiopronin), or captopril. These medications lower cystine concentration.
Patients with cystine stones must drink much more fluid than patients with other stones -- at least 4 quarts of water a day.
Other Treatments
Surgery is usually needed if:
- The stone is too large to pass on its own
- There are signs that the stone is growing
- The stone is blocking the urine flow
- It is causing a urinary tract infection or kidney damage
Today, treatments for stones are much less invasive than in the past. Major surgery is performed in less than 2% of patients.
Stone removal procedures:
- Extracorporeal shock wave lithotripsy (SWL) is used for small stones (smaller than 2 centimeters, or about three-quarters of an inch) that occur in the upper part of the ureter and do not pass on their own. Approximately 50-60% of stones are less than 10 mm in diameter and are quite responsive to SWL. Lithotripsy might even be safe and effective for patients whose stones are associated with malformed kidneys, although such patients are at higher risk for stone recurrence and should be carefully monitored. SWL takes less time to perform and requires a shorter hospital stay than percutaneous nephrolithotomy.
- Ureteroscopy is generally the best procedure for stones in the lower urinary tract, although lithotripsy is also usually feasible and patients ordinarily prefer it.
- Percutaneous nephrolithotomy (PCNL) can be used for large stones in the upper urinary tract, when SWL or ureteroscopy fails, for kidney transplant patients, or when the kidneys or surrounding areas are malformed. PCNL may produce better clearance of moderate size stones (10 - 20 mm) than SWL. PCNL is the preferred procedure for drug-resistant cystine stones, which are usually also resistant to shock wave therapy.
- Standard open surgery (nephrolithotomy) may be required if these procedures fail or are not appropriate, or in special cases, such as when the patient is very obese.
Most procedures are more effective for calcium and uric acid stones and less effective for struvite and cystine stones, although new techniques may be improving their effectiveness on all stones.
Extracorporeal Shock Wave Lithotripsy
Extracorporeal shock wave lithotripsy (SWL) is a technique that uses sound waves (ultrasound) to break up simple stones in the kidney or upper urinary tract. ("Extracorporeal" means "outside the body," and "lithotripsy" means stone-breaking.) SWL is not used for cystine stones. The procedure generally does not work for stones larger than 3 centimeters in diameter (which is slightly over an inch). SWL can often be done on an outpatient basis with limited anesthesia such as IV sedation and topical agents.
There are several variations of SWL. The following is a typical procedure:
- The patient is positioned in a water bath. (In some procedures the patient lies on a soft cushion.)
- The procedure uses ultrasound to generate shock waves that travel through the skin and body tissues until they hit the dense stones. (The doctor pinpoints the stone during treatment by using x-rays or ultrasound.)
- The shock waves crush the stones into tiny sand-like pieces that usually pass easily through the urinary tract.
The shattered stone fragments may cause discomfort as they pass through the urinary tract. If so, the doctor may insert a small tube called a stent through the bladder into the ureter to help the fragments pass. This practice, however, does not usually speed up passage of the stones and is not used routinely.
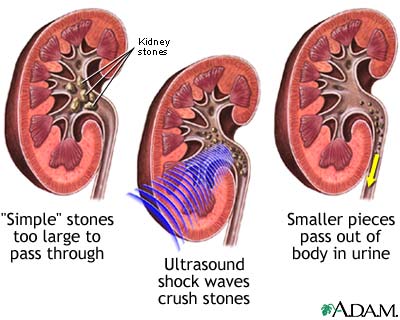
SWL has a 50 - 90% success rate, depending on the location of the stone and the surgeon's technique and experience. SWL is not as effective as percutaneous nephrolithotomy for stones in the lower kidneys, but it sometimes reduces the length of treatment and the hospital stay. Recovery time is short. Most people can resume their normal activities in a few days.
SWL is generally safe, and has few complications. If they do occur, complications may include:
- Blood in the urine, the most common complication, may last for a few days after treatment. To reduce the chances of bleeding, doctors usually tell patients to avoid taking aspirin and other NSAIDs (which can promote bleeding) for 7 - 10 days before the treatment.
- Bruising and minor discomfort due to the shock waves are common in the back or abdomen.
- Sometimes the stone does not completely break up with one treatment, and additional treatments may be required. Inability to pass stone fragments may also be a particular problem in patients who have cysts or other kidney problems.
- SWL may sometimes produce kidney damage.
SWL appears to be safe for children. Experts recommend using the least amount of shocks and impact possible in young people. If more than one treatment is needed, the patient should wait at least 15 days before having the next treatment.
Ureteroscopy
Ureteroscopy may be used for stones in the middle and lower ureter. Because it uses smaller instruments, this procedure can be done successfully in children.
During ureteroscopic stone removal:
- The patient receives a general anesthetic, though no incision is required for the procedure.
- The surgeon passes a small fiberoptic instrument called a ureteroscope through the urethra and bladder into the ureter.
- The surgeon locates the stone or stones.
- The urologist can use a laser to break up the stones, or remove them with a basket, grabber, or suction tool.
- The surgeon may decide to leave a small tube, or stent, in the ureter for a few days after treatment, to help the lining of the ureter heal.
Ureteroscopy achieves a higher stone removal rate than SWL, but it also has a higher risk of complications. In some cases, large stones are not broken up into small enough pieces. This can result in a blockage of the urinary tract and possible kidney damage.
Imaging tests, such as ultrasound or spiral CT, are useful within 3 months to check for residual stones, and a second procedure may be required. The risk of complications is highest when the procedure is performed by less experienced surgeons, or if stones are found in the kidney. The risk for perforation of the ureter increases the longer the procedure takes.
Percutaneous Nephrolithotomy
Percutaneous nephrolithotomy (PCNL) may also be used to treat kidney stones. It is often considered when SWL is not available or the patient is not a candidate for it (such as if the stone is very large, in a difficult to reach location, or is a cystine stone). PCNL is preferred over SWL for stones that have remained in the ureter for more than 4 weeks. PCNL is recommended for stones greater than 20 mm and perhaps for moderate size stones as well (10 - 20 mm).
PCNL is more effective than SWL for patients who are severely obese, and it appears to be safe for the very elderly and the very young. Success rates are very high for kidney stones and for ureteral stones; however, success may vary based on the technique used and the specific patient. For example, success rates are slightly lower in children, although the procedure can be done safely in young patients. Long-term effects are unknown.
A typical procedure is as follows:
- The surgeon makes a tiny incision in the skin and creates a channel directly into the kidney.
- The surgeon then inserts an instrument called a nephroscope through the channel.
- The stone is located and removed. If it is large, it is destroyed using ultrasound, lasers, or other devices. The surgeon then removes the fragments. An advantage of PCNL over SWL is that the surgeon is able to remove the stone fragments directly, instead of relying on their natural passage from the kidney.
- Generally, patients stay in the hospital for 3 - 5 days.
- Either a small device called a nephrostomy tube left in the kidney for drainage or a ureteral stent that keeps the ureter open may be used during the healing process. Both will be removed at some point after surgery. If neither is needed, the hospital stay may be shorter and there may be less pain.
Devices Used to Destroy Stones. For large stones, some type of energy-delivering device may be needed to break the stone into small pieces. These are referred to as intracorporeal lithotripsy devices (meaning stone breakers within the body), and may include:
- Ultrasound is currently the preferred method. It results in a stone-free rate of more than 90%. A rigid nephroscope delivers the ultrasound waves.
- Pneumatic (compressed air) lithotripsy uses a probe that comes in direct contact with a stone. Compressed air causes a piston to collide rapidly with the probe, and the result is a "jackhammer" action that breaks up the stone. However, this method can send stone fragments into other parts of the urinary tract.
- A more recent device uses a combination pneumatic probe and ultrasound. It produces stone-free rates of over 80%. It may prove to be superior to ultrasound alone, and it is effective against stones of all types.
- The holmium laser uses a flexible nephroscope to literally melt the stones. This laser destroys up to 100% of all types of stones and it has an excellent safety record. It should be used sparingly, however, and with particular caution on large uric acid stones until more is understood about its effect. (Another device, the erbium: YAG laser shows promise for lithotripsy, but is not currently in clinical use.)
Complications. Advances in technology have reduced the number and severity of complications related to
PCNL in recent years. Bleeding during surgery is the most common complication. Post-operative bleeding occurs in about 1% of PCNLs. Tears and injury to nearby organs or structures may also occur. Scarring of the tissue is one possible complication, but studies indicate that this scarring does not impair kidney function. Up to a third of patients experience fever after PCNL.
Because the procedure uses large volumes of fluid, fluid overload is a potential problem, particularly in children or patients with heart disease.
Infection may occur in some patients. Other serious complications may include a collapsed lung and injuries to areas outside the kidney (but within the operative area), such as the abdomen or chest, but occurrence is extremely rare.
Open Surgery (Nephrolithotomy)
Open surgery is the least common method for removing stones. It is only performed in a very small percentage of patients today. Called nephrolithotomy, it involves making incisions through the patient's flank and into the kidney. The surgeon will cool the kidneys using ice. X-rays taken during the procedure help locate the stone. The surgeon will isolate the arteries supplying the kidneys to ensure they are not harmed during the surgery. The surgeon will then locate and remove the stone. The surgeon will also correct any blockage in the affected area.
This surgery is very invasive and therefore is only used for:
- Patients with very large or complex stones that cannot be removed safely using less invasive measures
- Very obese patients
- Patients who have kidneys with anatomical abnormality or obstruction
- Patients undergoing open surgery for another condition
Some centers report success with extracorporeal shock wave lithotripsy in patients who would normally be nephrolithotomy candidates. Therefore, even these patients should discuss other options with their surgeon and seek advice from experienced centers.
The procedure is not appropriate for patients with:
- Bleeding or clotting disorders
- Untreated widespread infection
- Severe and chronic kidney disease (unless removing the stone will improve kidney function)
Complications
Between 70 and 90% of crystals remain tiny enough to travel through the urinary tract and leave the body in the urine without being noticed. When they do cause symptoms, however, kidney stones have been described as one of the most painful disorders to afflict humans. The pain they cause is sometimes called renal colic. ("Renal" means "kidney.")
Effects on the Urinary Tract and Kidneys
Obstruction and Infection. Although kidney stones often lead to obstruction (blockage) of the urinary tract, the blockage is usually temporary and causes no lasting damage. In some cases, however, particularly if the obstruction progresses with no symptoms, infection may occur, which can be serious and need immediate attention.
Chronic Kidney Disease. People with kidney stones face a higher risk for chronic kidney disease, particularly if they also have diabetes, high blood pressure, or frequent urinary tract infections. Having chronic kidney disease, in turn, can increase the risk for a heart attack. Researchers have found that in general, kidney stones increase the risk for a heart attack by more than a third (as well as the risk for certain other disorders), independent of their effect on chronic kidney disease.
Kidney Failure. It is very rare for kidney stones to cause kidney failure. However, some people have risk factors that make them more vulnerable to this serious complication, such as:
- Very frequent stone recurrences (such as in people with cystine stones or other inherited forms of kidney stone disorders)
- Episodes of urinary tract infections with obstruction, a particular risk with struvite stones
- A history of having many procedures for kidney stones
- Greater size of the kidney stone gravel
Long-Term Outlook: Risk for Recurrence
Without treatment, calcium stones recur in 40% of patients within 5 years of the first attack, and in 75% of patients within 20 years. The individual risk for recurrence, however, varies depending on the stone and the underlying condition. For example, a 15-year-old with inherited cystine stones has a very high risk for recurrence, while a middle-aged man with a first calcium oxalate stone has a good chance of never passing another stone.
Prevention
Anyone who has had kidney stones should try to prevent a recurrence. Some general prevention tips include:
- Increase fluid intake, restrict sodium, and reduce protein intake
- Get more potassium
- Try to correct any dietary habits that cause acid or alkaline imbalances in the urine, which promotes stone formation
Eating a high-calcium diet does not appear to increase the risk for kidney stones, as long as the diet also contains plenty of fluids, potassium, and phosphate. (Increasing calcium alone may pose a modest risk for stones.)
Because different kidney stone types may require specific dietary changes, patients should work with their doctors to develop an individualized plan. Nutritional considerations are very important in preventing recurrences, and patients should comply with the proper diet.
Fluids (Water, Juice, and Other Beverages)
Of all the preventive recommendations, drinking enough fluids is the most important guideline for people with any type of kidney stones.
- In general, patients with calcium or uric acid stones should drink at least 10 full glasses of fluid each day (at least half should be water). They should drink one glass with each meal and drink fluids at night, even if they have to get up during the night to go to the bathroom. Fluid intake should produce at least two-and-a-half quarts of urine each day.
- To prevent cystine stones, patients should drink even more water -- more than a gallon, or 16 8-ounce cups, every day. Patients should drink this amount at regular intervals throughout the day and night.
In all cases, patients need more fluid after exertion and during times of stress. If they drink enough, the urine should be pale and almost watery, not dark and yellow.
Water. Water hardness (meaning how much calcium is in the water) generally plays only a small role in stone formation. By far, the amount of fluid intake is most important in preventing stones.
Juices. Other beverages have various effects, depending on the type of stone:
- Lemon Juice: Drinking one-half cup of pure lemon juice (enough to make 8 glasses of lemonade) every day raises citrate levels in the urine, which might protect against calcium stones. (While orange juice also increases citrate levels, it does not lower calcium and it raises oxalate levels. Therefore, it is not recommended.)
- Cranberry and Apple Juice: Apple and cranberry juice contain oxalates, and both have been associated with a higher risk for calcium oxalate stones. Cranberry juice has properties that may increase the risk for both calcium oxalate and uric acid stones. On the other hand, cranberry juice helps prevent urinary tract infections, so it may be helpful for reducing the risk for struvite and brushite stones. (These stones are far less common, however.)
- Grapefruit Juice: Several studies have found that drinking grapefruit juice might increase the risk for stones.
Other Beverages and Their Effects on Stone Formation.
- Soft Drinks. Patients with stones should avoid cola drinks that contain phosphoric acid, because they can severely reduce citrate levels in the urine. However, citrus-based sodas (such as 7 Up and Sprite) are high in citrate, which might help prevent stones from forming, particularly in patients with low citrate in their urine, or who have a tendency to form uric acid stones.
- Alcohol. Wine may protect against kidney stones. However, it is important to remember that beer and other alcoholic beverages also contain purines, which may increase the risk for the less common uric acid stones in susceptible people. Binge drinking increases uric acid and the risk for stones.
- Coffee and Tea. Some research has reported a lower risk for stones in people who drink tea and both regular and decaffeinated coffee.
Low-Salt and Low-Protein Diets
A low-sodium, low-to-moderate protein diet containing normal levels of calcium can help reduce the recurrence of stones compared to a low-calcium only diet.
Salt Restriction. Because salt intake increases the amount of calcium in urine, patients with calcium stones should limit their sodium intake to 1,500 mg or less a day. Sodium may also increase levels of urate, the crystalline substance that can trigger the formation of recurrent calcium oxalate stones.
Protein Restriction. Protein increases uric acid, calcium, and oxalate levels in the urine, and reduces citrate levels. Diets high in protein, particularly meat protein, have been consistently connected with kidney stones. (Meat protein has a higher sulfur content and produces more acid than vegetable protein.)
Whether restricting meat protein alone without restricting sodium has any protective value is unknown. Most studies to date have found no difference in stone development between people with low and normal protein diets.
Although the precise role of dietary protein in kidney stones needs further clarification, it is reasonable for everyone to consume meat protein in moderation. People with struvite stones who need to reduce phosphates in their diets should also cut down on protein.
DASH Diet. The same diet that is recommended to control blood pressure might also reduce the risk of kidney stones. The DASH diet, which is high in fruits and vegetables and low in animal protein, appears to reduce the incidence of kidney stones by as much as 40 - 50%.
Role of Calcium
Calcium from Foods. Dietary calcium recommendations for kidney stone prevention need to be determined on an individual basis. A doctor will suggest calcium guidelines based on a patient's age, gender, body size, and type of stone. General recommendations for daily dietary calcium intake are: 1,300 mg for teenagers, 1,000 mg for men and women ages 19 - 50, and 1,200 mg for women after age 50 and men after age 70. Most studies indicate that people who eat the recommended amount of dietary calcium (found in milk, yogurt, and cheese) have a lower chance of stone recurrence than those who eat a low-calcium diet. Therefore, a diet containing a normal amount of calcium, but reduced amounts of animal protein and salt may protect against stones better than a low-calcium regimen.
Calcium Restriction in Certain Cases. Some patients, such as those whose stones are caused by genetic defects in which the intestine absorbs too much calcium, may need to limit calcium intake. More studies are needed to define this group precisely.
Fiber-Rich Foods and Their Compounds
Fiber may be beneficial for people with kidney stones. In addition, some fiber-rich foods may contain compounds that help protect against kidney stones. A wide variety of high-fiber plant foods contain a compound called phytate (also called inositol hexaphosphate, InsP6, or IP6), which appears to help prevent the crystallization of calcium salts, both oxalate and phosphate. Phytate is found in legumes and wheat and rice bran. (Soybeans are also rich in phytate, but they are also very high in oxalates, so the overall effects of soy on kidney stones are not clear.)
Purine Restriction in People at Risk for Uric Acid Stones
A high intake of purines can increase the amount of uric acid in the urine. Those at risk for uric acid stones should reduce their intake of foods and beverages that contain purines.
Some diet and lifestyle changes that may help prevent uric acid stones:
- Avoid alcohol, anchovies, sardines, oils, herring, organ meat (liver, kidney, and sweetbreads), legumes (dried beans and peas), gravies, mushrooms, spinach, asparagus, cauliflower, and baking or brewer's yeast.
- Limit how much meat you eat at each meal.
- Avoid fatty foods such as salad dressings, ice cream, and fried foods.
Oxalate Restriction in Hyperoxaluria
People who have hyperoxaluria will be advised to limit the amount of oxalate in their diet.
- Foods high in oxalic acid include beets, soy, black tea, chenopodium, chocolate, cocoa, dried figs, ground pepper, lamb, lime peel, nuts, parsley, poppy seeds, purslane, rhubarb, sorrel, spinach, and Swiss chard.
- Foods containing moderate amounts of oxalates include beans (green and wax), blackberries, blueberries, carrots, celery, coffee (roasted), concord grapes, currants, dandelion greens, endive, gooseberries, lemon peel, okra, green onions, oranges, green peppers, black raspberries, strawberries, and sweet potatoes.
Role of Fats
Certain fats may play a beneficial or harmful role in specific cases of kidney stones.
Restricted Fats in Patients with Stones Associated with Bowel Disease. Patients who have stones associated with short-bowel syndrome should eat foods with lower amounts of fats and oxalates. If patients with short-bowel syndrome eat too much fat, calcium may bind to unabsorbed fat instead of to oxalates, increasing oxalate levels and raising the risk of stone formation.
Fish Oil. Omega-3 fatty acids, found in oily fish like mackerel, salmon, and albacore tuna, have many health benefits, but the most current evidence suggests they do not help prevent kidney stones.
Role of Vitamins
Vitamin B6. Vitamin B6, or pyridoxine, is used to treat people with primary hyperoxaluria, a severe inherited disorder. Patients should not try to treat themselves with vitamin B6. Very high doses (500 - 2,000 mg daily over long periods of time) can cause nerve damage. Food sources of vitamin B6 include meats, oily fish, poultry, whole grains, dried fortified cereals, soybeans, avocados, baked potatoes with skins, watermelon, plantains, bananas, peanuts, and brewer's yeast.
Vitamin C. Ascorbic acid (vitamin C) may change in the body to tiny crystals, called oxalates. These crystals do not dissolve. People with hyperoxaluria (too much oxalate in the urine) should avoid vitamin C supplements. Even for men with normal oxalate levels, higher consumption of vitamin C (more than 1,000 mg a day) may increase kidney stone risk.
Stress Management Techniques
Because of an association between stress and kidney stones, relaxation and stress management techniques may also be beneficial.
Preventing Recurrence
Dietary Considerations. People with kidney stones appear to be more sensitive to certain foods than people who do not form kidney stones. Therefore, vulnerable people should make specific changes in their diet. They should work with their doctors to develop a dietary plan that fits their individual situation. Drinking plenty of fluids is important for preventing a recurrence of any kidney stone.
Indications for Drug Treatments. If dietary treatments fail, drug therapy may be helpful. A number of drugs are available to prevent recurrences of calcium oxalate and other stones. Medications that inhibit the formation of stones include allopurinol, thiazide, potassium citrate, and potassium-magnesium citrate. In addition, drug treatments can sometimes help prevent other complications related to stones, such as osteoporosis.
Correcting Underlying Conditions Known to Cause Kidney Stones. It is also important to treat and correct, if possible, any underlying disorder that may be causing stones to form. Such disorders include distal renal tubular acidosis, hyperthyroidism, sarcoidosis, and certain cancers. To prevent calcium stones that form in hyperparathyroid patients, a surgeon may remove the affected parathyroid gland (located in the neck).
Resources
- http://kidney.niddk.nih.gov/ -- National Kidney and Urologic Diseases Information Clearinghouse
- www.auanet.org -- American Urological Association
References
Christian C, Thorsten B. The preferred treatment for upper tract stones is extracorporeal shock wave lithotripsy (ESWL) or ureteroscopic pro ESWL. Urology. 2009;74(2):259-262.
Deem S, Defade B, Modak A, Emmett M, Martinez F, Davalos J. Percutaneous nephrolithotomy versus extracorporeal shock wave lithotripsy for moderate sized kidney stones. Urology. 2011;78(4):739-43.
Eisner BH, Asplin JR, Goldfarb DS, Ahmad A, Stoller ML. Citrate, malate and alkali content in commonly consumed diet sodas: implications for nephrolithiasis treatment. J Urol. 2010;183(6):2419-2423.
Ferrandino M, Peitrow P, Preminger G. Evaluation and Medical Management of Urinary Lithiasis. In: Wein AJ ed: Campbell-Walsh Urology, 10th. ed. Philadelphia, PA: Saunders Elsevier. 2011:chap 46
Maalouf NM, Tondapu P, Guth ES, Livingston EH, Sakhaee K. Hypocitraturia and hyperoxaluria after Roux-en-Y gastric bypass surgery. J Urol. 183(3):1026-1030.
Matlaga B, Lingeman J. Surgical Management of Upper Urinary Tract Calculi. In: Wein AJ ed. Campbell-Walsh Urology, 10th. ed. Philadelphia, PA: Saunders Elsevier. 2011:chap 48
Miller NL, Evan AP, Lingeman JE. Pathogenesis of renal calculi. Urol Clin North Am. 2007; 34(3):295-313.
Monk RD, Bushinsky DA. Kidney Stones. In: Kronenberg HM, Melmed S, Polonsky KS, Larsen PR, eds. Williams Textbook of Endocrinology. 12th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 30.
Pietrow PK, Preminger GM. "Evaluation and Medical Management of Urinary Lithiasis." In: Wein AJ, Kavoussi LR, Novick AC, et al. (eds.) Wein: Campbell-Walsh Urology, 9th ed. Philadelphia, PA: Saunders; 2007.
Rule AD, Roger VL, Melton LJ 3rd, Bergstralh EJ, Li X, Peyser PA, et al. Kidney stones associate with increased risk for myocardial infarction. J Am Soc Nephrol. 2010; 21(10):1641-1644.
Saucier NA, Sinha MK, Liang KV, Krambeck AE, Weaver AL, Bergstrath EJ, Li X, et al. Risk factors for CKD in persons with kidney stones: a case-control study in Olmsted County, Minnesota. Am J Kidney Dis. 2010;55(1):61-68.
Semins MJ, Matlaga BR, Shore AD, Steele K, Magnuson T, Johns R, Makary MA. The effect of gastric banding on kidney stone disease. Urology. 2009;74(4):746-749.
Shen P, Jiang M, Yang J, et al. Use of ureteral stent in extracorporeal shock wave lithotripsy for upper urinary calculi: a systematic review and meta-analysis. J Urol. 2011;186(4):1328-35. Review.
Sinha MK, Collazo-Clavell ML, Rule A, et al. Hyperoxaluric nephrolithiasis is a complication of Roux-en-Y gastric bypass surgery. Kidney International. 2007;72:100-107.
Srisubat A, Potisat S, Lojanapiwat B, Setthawong V, Laopaiboon M. Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIS) for kidney stones. Cochrane Database Syst Rev. 2009 Oct 7:(4):CD007044.
Taylor EN, Fung TT, Curhan GC. DASH-style diet associates with reduced risk for kidney stones. Am J Soc Nephrol. 2009;20(10):2253-2259.
Wang J, Zhao C, Zhang C, Fan X, Lin Y, Jiang Q. Tubeless vs standard percutaneous nephrolithotomy: a meta-analysis. BJU Int. 2012;109(6):918-24. Review.
Wolf JS. Percutaneous Approaches to the Upper Urinary Tract Collecting System. In: Wein AJ ed: Campbell-Walsh Urology, 10th. ed. Philadelphia, PA: Saunders Elsevier. 2011:chap 47
Worcester EM, Coe FL. Calcium kidney stones. N Engl J Med. 2010; 363:954-963.
|
Review Date:
8/27/2012 Reviewed By: Reviewed by: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M. Health Solutions, Ebix, Inc. |






